As one of the leading providers of labels and wristbands to the healthcare industry, we understand how critical positive patient identification is to patient safety. Identifying patients correctly at each point on their healthcare journey helps reduce potentially fatal treatment and medication errors. The process of positively identifying a patient also offers healthcare organizations an opportunity to build relationships and improve communication with patients and families.
Clearly, the topic of positive patient identification is a top of mind for healthcare organizations nationwide. The Joint Commission has included it as a National Patient Safety Goal since 2003. The National Quality Forum also lists wrong-patient mistakes as serious reportable events and also considers patient identification as a high-priority area for measuring health information (IT) safety.
The Consequences of Patient ID Errors
Unfortunately, patient identification errors still occur and the consequences can be catastrophic. The following are all real examples drawn from a database maintained by ECRI, an independent nonprofit that strives to improve the safety, quality and cost-effectiveness of healthcare worldwide
- A patient in cardiac arrest was not resuscitated because the care team accessed the wrong patient’s record – which included a do-not-resuscitate order.
- An infant received breast milk intended for a different infant. The mother who produced the breast milk had the hepatitis B virus, meaning the infant who received the milk had to be treated with hepatitis B immune globulin.
- Two patients with the same first name were scheduled for cataract surgery. The wrong patient was brought into the operating room and received the lens implant intended for the other patient.
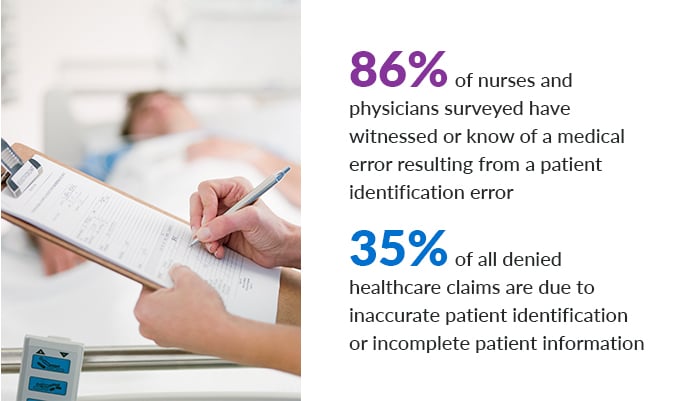
Errors of this nature are all too common. In a report published by the Ponemon Institute, 86% of nurses and physicians surveyed have witnessed or know of a medical error resulting from a patient identification error. These errors also have a direct financial impact on healthcare organizations, even without the obvious malpractice implications. An estimated 35% of all denied healthcare claims are due to inaccurate patient identification or incomplete patient information.
According to the Ponemon Institute, 35% of all denied claims are the direct result of inaccurate patient identification or incomplete patient information, costing the average healthcare facility $1.2 million per year. This is not entirely surprising. AHIMA found that up to 12% of all electronic health records (EHR) are duplicates, resulting vast amounts of missing health information and inadvertent mingling of different patients’ records.
12 Tips That Promote Positive Patient Identification
Fortunately, there are many things that can be done to promote positive patient identification, or PPID for short. We’ve assembled a list of 12 tips to help you protect your patients – and your healthcare organization – from patient identification errors. While most are now common knowledge (or even common sense) for healthcare professionals, PPID is a topic worthy of frequent reminders.
PPID Tip #1: Use two forms of identification
Always use at least two separate methods of identifying a patient, such as the patient’s name and date of birth. Do not use patient room number as an identifier.
PPID Tip #2: Involve the patient
Ask patients to identify themselves before receiving medication or treatment and encourage patients to participate in all stages of the process. If possible, ask patients or family members to verify identifying information to ensure its accuracy.
PPID Tip #3: Listen for questions
If a patient or family asks a question or expresses confusion about something related to patient identification, stop and listen. This may be the warning you need to prevent an error.
PPID Tip #4: Ask, don’t confirm
Use specific language to ask a patient to identify themselves. Do not ask them to confirm their name. Instead say, “Please tell me your name.”
PPID Tip #5: Standardize your methods
If you are part of a multi-facility healthcare organization, take steps to standardize your approach to patient identification among all of the facilities within the system. For example, standardize how names are displayed in electronic health records. Then, audit your policies and processes regularly to discover any potential system-wide risks.
PPID Tip #6: Have a plan for no name, same name
Provide clear protocols to staff members for identifying patients who lack identification, and for distinguishing the identity of patients with the same name.
PPID Tip #7: Snap a photo
Update your protocols to include patient photos, such as on patient wristbands. The use of patient photos is still in the minority among hospitals but it’s a powerful defense against patient identification errors.
PPID Tip #8: Don’t leave without labeling
Always label blood and other specimens in the presence of the patient. It’s too easy to forget which label goes with which specimen.
PPID Tip #9: Pay attention to your little voice
Establish clear protocols for questioning test results or findings when they are not consistent with the patient’s clinical history. If something doesn’t look right, it probably isn’t.
PPID Tip #10: Get it right from the start
Create clearly defined policies and procedures for the registration process to prevent patient registration errors from affecting care later in the visit. Devote adequate staffing resources to the registration team so they don’t feel rushed, which is often a source of errors.
PPID Tip #11: Embrace digital technology
Implement automated healthcare technology systems – EHRs, computerized provider order entry, bar coding, RFID, digital informed consent tools, physiologic monitors, e-prescribing, etc. – wherever possible. Doing so is proven to decrease the potential for patient identification errors.
PPID Tip #12: Discuss and learn
Foster a culture where patient identification errors can be called out and discussed without fear of retribution. Every error offers an opportunity for learning and improvement.
Taylor Healthcare: Leading the Way in Positive Patient Identification
Taylor Healthcare has been managing healthcare information and communications for more than 100 years. We offer a full range of quality patient identification solutions tailored to the healthcare environment. Led by our seasoned healthcare specialists, we offer both traditional wristbands and labels as well as technology-enabled solutions that integrate barcodes, patient photos and demographics. The result is a patient identification strategy that empowers you to:
- Establish positive patient identification from admission through discharge
- Assure patient comfort and safety
- Achieve Joint Commission National Patient Safety Goals
- Comply with HIPAA requirements
- Improve the efficiency of your admissions and clinical staff